Our health insurance experts can get most of our clients covered by their health insurance plan for their permanent hair removal treatment.
"How Can I Get My Electrolysis Covered By Insurance?"
Electrolysis is permanent hair removal. It is also one of the most essential forms of gender-affirming care for many trans women, trans men preparing for phalloplasty, and nonbinary people pursuing surgery prep hair removal.
One question rises above all others: “How can I get electrolysis insurance coverage?”
If you have asked this, you are far from alone. Many people search online and find conflicting answers. Some insurers classify electrolysis as cosmetic. Others treat it as medically necessary care for gender dysphoria. Many insurance representatives are unfamiliar with their own guidelines or national gender-affirming care policies. When you ask is electrolysis covered by insurance, you step into a landscape shaped by policies, diagnostic codes, regional differences, and inconsistent staff training.
At Real You Electrolysis, we support hundreds of trans clients across Washington and Oregon. Our clinics in Vancouver and Lakewood work with insurers daily. We talk to representatives. We navigate plan rules. We advocate for approval. We see patterns that individual clients cannot see on their own. This guide draws from that experience. It applies specifically to Washington and Oregon, yet much of it is useful nationwide because many insurers operate under national policies.
A Complete Guide To Insurance Coverage for Hair Removal
This guide is designed to answer every common (and uncommon) question related to electrolysis insurance coverage, including:
- Does insurance cover electrolysis for transgender women?
- Does insurance cover facial electrolysis?
- Does insurance cover genital electrolysis?
- Does insurance cover electrolysis before vaginoplasty?
- Does insurance cover electrolysis before phalloplasty?
- Does insurance cover electrolysis for graft sites?
- Does Medicaid cover electrolysis?
- Does Medicare cover electrolysis?
- Does insurance cover electrolysis in restrictive states?
- How do you get insurance to approve electrolysis?
- What documentation do you need for electrolysis insurance claims?
- What happens when insurance calls electrolysis “cosmetic”?
- How long do electrolysis insurance approvals take?
- What should you do if insurance denies electrolysis?
This insurance guide is intended as a comprehensive answer to your electrolysis insurance coverage questions, based on three years of working with insurance providers to cover permanent hair removal for our clients.
Understanding Whether Electrolysis Is Covered by Insurance
Insurance policies treat different categories of electrolysis hair removal differently. This is the root of almost all confusion around the question: does insurance cover electrolysis hair removal? Most plans examine electrolysis in three separate groups:
- Facial electrolysis
- Electrolysis genital surgery preparation for vaginoplasty or phalloplasty
- Electrolysis on torso, chest, graft sites, or other non-facial areas
How each category is handled depends on diagnosis, documentation, medical necessity, insurer guidelines, and state-level gender-affirming care protections.
Many plans approve surgery preparation electrolysis consistently, approve facial electrolysis with documentation, and approve torso or graft-site electrolysis on a case-by-case basis. This is why people searching “is electrolysis covered by insurance” often receive mixed replies online.
Why Electrolysis Is Medically Necessary in Gender-Affirming Care
Electrolysis is the only method recognized by the U.S. Food and Drug Administration (FDA) as permanent hair removal. Laser is categorized as permanent hair reduction, meaning it cannot guarantee full destruction of the follicle.
For gender-affirming care, the permanence of hair removal matters in two ways:
1. Daily functioning and gender dysphoria relief
Facial hair can affect safety, emotional wellbeing, confidence, and social ease. Permanent removal reduces triggers of dysphoria and supports daily mental health. When insurers evaluate does insurance cover electrolysis for facial areas, medical necessity is often established through the connection between facial hair and gender dysphoria.
2. Surgical safety for vaginoplasty and phalloplasty
Hair regrowth in surgical areas could lead to complications, sub-optimal results. Surgeons want certainty that no hair grows inside internal surgical sites, or within the boundaries of the affected area. For vaginoplasty, this includes the scrotal area, perineum, and mons. For phalloplasty, this includes graft sites such as the forearm or thigh.
Laser cannot guarantee zero regrowth. Electrolysis can.
Because of this, pre-surgical electrolysis genital hair removal is widely recognized as medically necessary.
This is why some insurers who might deny laser frequently approve electrolysis once they receive the surgeon’s requirements.
But also, be careful – some insurance plans DO cover both electrolysis and laser hair removal, because they may not know the difference – and once they approve one they might not approve the other – they do not often approve both for the same patient or in the same time frame.
Because of this, pre-surgical genital electrolysis is widely recognized as medically necessary.
This is why some insurers who might deny laser frequently approve electrolysis once they receive the surgeon’s requirements.
But also, be careful – some insurance plans DO cover both electrolysis and laser hair removal, because they may not know the difference – and once they approve one they might not approve the other – they do not often approve both for the same patient or in the same time frame. So if you get laser hair removal insurance coverage, you might be limiting your access to electrolysis insurance coverage.
Does Insurance Cover Electrolysis for Transgender Women?
In many cases, yes. Electrolysis insurance coverage approval depends on the category of treatment:
- Facial hair removal: often approved with documentation
- Electrolysis genital surgery prep: almost always approved
- Torso or other areas: variable
Approval is strongest when the client has:
- A diagnosis of gender dysphoria
- A mental health provider’s letter recommending electrolysis
- A primary care or hormone-prescribing provider’s letter
- Clear identification of the specific areas requiring treatment
- A surgeon’s letter when surgery prep is involved
In our experience, most insurance carriers in Washington and Oregon approve at least one of these categories for transgender women.
Does Insurance Cover Facial Electrolysis?
Often, yes — especially in states with strong gender-affirming care protections like Washington and Oregon.
Facial electrolysis is evaluated for:
Impact on daily functioning
Impact on gender dysphoria
Safety concerns (misgendering risks, shaving injuries, or skin conditions)
Overall transition goals
Most insurers that approve facial electrolysis require:
- A diagnosis of gender dysphoria
- A mental health letter
- A primary care letter
- A clear treatment plan
Insurers known to approve facial electrolysis in OR/WA include:
- Kaiser Permanente
- Pacific Source
- Moda
- Blue Cross
- Oregon Health Plan
- Some Cigna plans
- Washington Medicaid
Coverage in other states varies depending on whether the state protects gender-affirming care, whether the insurer follows national guidelines, and whether the plan includes trans-inclusive benefits.
Does Insurance Cover Electrolysis for Vaginoplasty Prep?
Yes. Pre-surgical genital electrolysis is one of the most consistently approved forms of electrolysis across private insurance, Medicaid programs, and large national carriers. When surgeons state that permanent hair removal is mandatory before vaginoplasty, insurers typically approve it.
Areas that require clearance:
- Scrotal skin
- Top, sides and bottom of the phallus (penis)
- Perineum
- Mons pubis
Surgeons require electrolysis genital permanent hair removal to prevent hair growth inside the vaginal canal. Regrowth can cause infection, embedded hair, chronic irritation, and surgical complications. Because of this, insurers treat this category as medically necessary gender-affirming care
Does Insurance Cover Electrolysis for Transgender Men?
Does Insurance Cover Electrolysis for Phalloplasty Prep?
Often, yes.
For phalloplasty, hair must be removed from graft sites used to create the phallus. Common graft areas include:
- Radial forearm
- Anterolateral thigh
- Lower abdomen
- Upper thigh
Most insurers approve graft-site electrolysis once the surgeon confirms the necessity. The medical rationale is the same: hair regrowth inside a urological structure can create complications.
Documentation from the surgical program typically leads to approval.
Does Insurance Cover Electrolysis for Graft Sites?
Yes, frequently — when tied to gender-affirming surgery.
Coverage depends on the surgical letter and identification of the exact graft site.
Large carriers like Kaiser, Blue Cross, Aetna, and Cigna often approve graft-site electrolysis even when they deny other cosmetic services.
Is Electrolysis Hair Removal Covered by Medicaid?
Washington State (Apple Health)
In Washington, Apple Health frequently covers:
- Facial electrolysis for gender dysphoria
- Surgery preparation electrolysis
- Electrolysis for graft sites
- Electrolysis on torso or chest when medically documented
Washington State has robust trans-inclusive healthcare protections, and Apple Health follows these protections.
Oregon (Oregon Health Plan / OHP)
OHP is one of the most trans-inclusive Medicaid programs in the country. It often covers:
- Facial electrolysis
- Genital surgery prep electrolysis
- Graft-site electrolysis
- Torso or chest electrolysis when medically necessary
Coverage in other states varies depending on whether the state protects gender-affirming care, whether the insurer follows national guidelines, and whether the plan includes trans-inclusive benefits.
Does Medicaid Cover Electrolysis Hair Removal Nationwide?
Medicaid policies vary widely. Some Medicaid programs explicitly exclude electrolysis insuramce coverage, while others approve it under gender-affirming care guidelines. Approval often depends on:
- State-level transgender healthcare protections
- Interpretation of medical necessity
- Documentation quality
- The presence of a surgeon’s letter
Because Medicaid differs by state, clients in restrictive states often call their Medicaid office and receive inaccurate information. Referring to the insurer’s national policy can sometimes override local interpretation.
Is Electrolysis Hair Removal Covered b Medicare?
Is electrolysis covered by Original Medicare?
No.
Unfortunately, Original Medicare does not cover electrolysis for any reason, including gender-affirming care.
This makes it important to plan ahead – especially if you’re in your fifties. Electrolysis has a great advantage over laser in that it’s permanent hair removal, but it CAN be a lengthy process. If you get on a weekly rhythm and you’re covered by health insurance, hair removal can become simply another aspect of your weekly routine. But if you don’t plan ahead, you may be in for a rude awakening when you turn 65. If you can, plan to be done with hair removal part of your transition long before that.
Is electrolysis covered by Medicare Advantage?
Sometimes.
Medicare Advantage plans behave more like commercial insurance, and some of these plans do approve electrolysis as gender-affirming care — especially surgery prep electrolysis.
Coverage varies by plan. If you are approaching age 65 and currently receiving electrolysis hair removal through Medicaid or commercial insurance, you may want to evaluate Medicare Advantage options carefully to preserve access.
How to Ask: Is Electrolysis Covered by My Insurance Plan?
Many representatives do not know their own rules. Some rely on outdated scripts that classify electrolysis as cosmetic. Some have never reviewed their company’s gender-affirming care guidelines.
The way you phrase your questions influences the accuracy of the answers you receive.
Below is a phone script designed to produce the clearest results:
A Phone Script to Ask Insurance Reps About Hair Removal Coverage
“Hello. I am calling to verify whether I have electrolysis insurance coverage under my plan.”
“I am receiving electrolysis for gender dysphoria as part of my transition.”
“I need to confirm whether facial electrolysis is covered by insurance.”
“I also need to confirm whether surgery preparation electrolysis is covered.”
“I will be completing pre-surgical genital electrolysis for a gender-affirming procedure.”
“Can you tell me what documentation you need from my providers?”
“Can you confirm which diagnostic codes are required when billing electrolysis?”
Precise phrasing prompts representatives to check the correct benefit category instead of defaulting to “cosmetic.”
Documentation You'll Need for Electrolysis Insurance Coverage
Documentation determines approval more reliably than phone calls.
When insurers ask is electrolysis covered by insurance, these items carry the most weight:
1. Mental health letter
This letter should include:
- Diagnosis of gender dysphoria
- Statement that electrolysis is part of gender-affirming care
- Recommendation for facial or surgical prep electrolysis
- Confirmation that permanent removal improves functioning
2. Primary care letter
This letter should include:
- Confirmation of gender dysphoria
- Summary of why electrolysis is medically necessary
- Identification of specific areas needing treatment
- Recommendation for surgery prep hair removal when applicable
Letters must usually be dated within the past 12–18 months.
3. Diagnostic codes
Plans often request:
- F64.0 (older terminology still used by systems), or
- Current gender dysphoria codes used by modern providers

How Insurance Decisions Are Made Behind the Scenes
When you call your plan and ask “is electrolysis covered by insurance?” the first answer you hear is not always the final answer. Representatives often rely on scripts or outdated internal categories. Electrolysis insurance coverage is decided by multiple layers within the insurer’s system, and the decision-makers at each layer have different levels of authority.
Understanding these layers helps you navigate the process more confidently.
1. The call-center representative
This is the person who answers the phone. They rely on:
- Pre-written scripts
- Database notes
- Default classifications (which often list electrolysis as cosmetic)
They rarely review the gender-affirming care chapter of the plan manual unless prompted.
If they say “cosmetic,” it often reflects:
- Lack of training
- Failure to check the correct benefit section
- Outdated internal terminology
This is why phrasing matters. Mentioning gender dysphoria, surgery preparation, or gender-affirming care guidelines often prompts them to check the correct policy.
2. The plan administrator
This is the department Real You Electrolysis usually communicates with when submitting claims and letters. Administrators:
- Review the mental health letter;
- Review the primary care letter;
- Verify diagnostic codes;
- Confirm that the requested areas match recognized medical necessity.
They often have more accurate information than call-center representatives.
3. The medical necessity reviewer or underwriter
This is usually the final decision-maker. They evaluate:
- Whether documentation supports gender dysphoria treatment
- Whether surgery preparation requires permanent hair removal
- Whether electrolysis meets safety thresholds for surgical success
Underwriters almost always approve pre-surgical genital electrolysis when the surgeon confirms that permanent removal is mandatory.
Understanding this structure helps explain why someone online may report a denial while another reports an approval under the same plan.
How Long Does Insurance Approval for Electrolysis Take?
Insurance timelines vary depending on:
- The insurer
- The type of electrolysis
- The quality of documentation
- Whether surgery is scheduled
Typical timelines for electrolysis insurance approval
Pre-surgical genital electrolysis hair removal
1–4 weeks
Approvals tend to be faster because surgeons require it. Plans prioritize this category due to the risk of complications if hair remains inside surgical sites.
Facial electrolysis
2–8 weeks
Timelines depend on whether the insurer requests additional documentation. Facial electrolysis may require more justification than surgery prep electrolysis.
Torso, chest, or graft-site electrolysis
2–8 weeks
Some plans request clarification on medical necessity for these areas unless they are tied to surgery.
Medicaid (Oregon or Washington State)
Usually faster than private plans once documentation is complete, as the coverage rules for trans-related services are well established in both states.
COMMON REASONS FOR INSURANCE DELAYS:
- The mental health and/or doctor letter is missing required language, dates, and signatures
- Diagnostic codes don’t match the plan’s requirements
- The representative misclassified electrolysis as cosmetic
- The insurer requests updated letters
- The claimant recently changed insurance
Submitting complete documentation through a clinic familiar with the system reduces delays significantly.
Electrolysis vs. Laser: Why Insurers Treat Them Differently
Something that puzzles many people are the different responses to electrolysis insurance coverage vs laser insurance coverage questions. Why are these methods of hair removal often met with different coverage outcomes, different responses from insurance reps?
The short answer is that insurers often deny laser and approve electrolysis.
Reasons insurers do not treat laser as medically equivalent:
- Laser is permanent hair reduction, not removal;
- Laser cannot guarantee full follicle destruction;
- Laser does not meet surgical safety requirements;
- Laser is ineffective on light, blond, gray, or red hair;
- Laser outcomes vary widely depending on skin and hair.
Why electrolysis is preferred by insurers for medical necessity:
- Electrolysis permanently destroys the follicle;
- Electrolysis works on all hair colors and skin tones;
- Surgeons rely on electrolysis for safe outcomes;
- Electrolysis prevents regrowth that can impair surgical sites
Some plans explicitly state that laser hair removal is not covered, while electrolysis may be approved under gender dysphoria treatment or gender-affirming care.
This distinction significantly affects individuals preparing for vaginoplasty or phalloplasty.
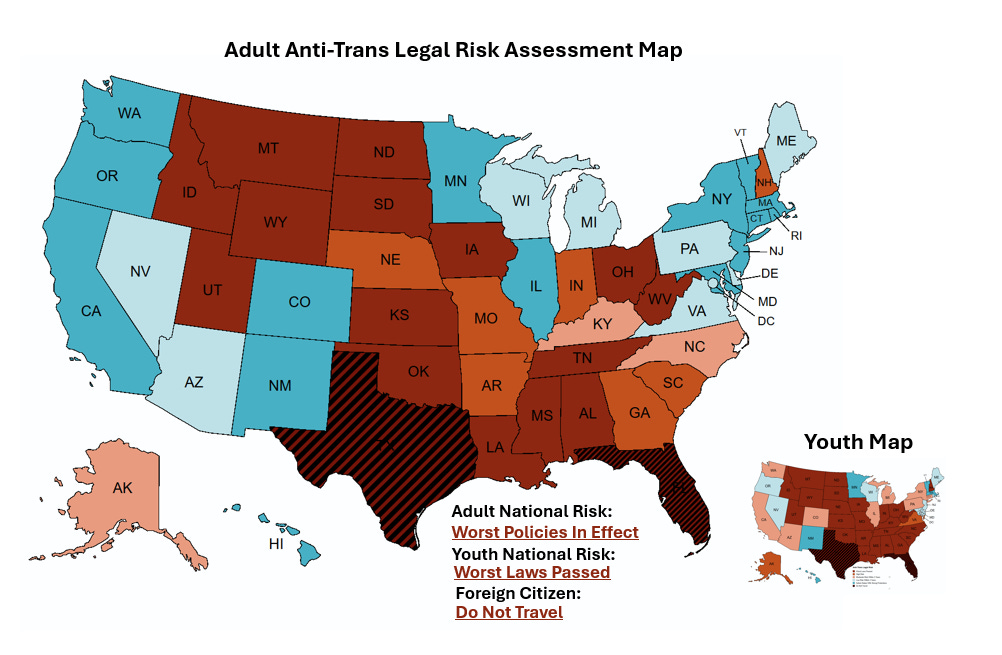
Insurance Coverage in Trans-Restrictive or Trans-Hostile States
As you can see in the map above, transgender legislation across the United States varies enormously from state to state.
In 2021, Washington passed 2SSB-5313, prohibiting health insurers from denying or
limiting coverage for gender affirming treatment (GAT) when care is medically necessary, and specifically forbidding the re-classification of “cosmetic” to such care.
While electrolysis insurance coverage might be available in New York, Delaware or Minnesota or Colorado, it is least likely to be offered in Texas or Florida.
Transgender folks in restrictive states often ask:
- “Does insurance cover electrolysis in my state?”
- “Why did my representative tell me no when the plan covers it nationally?”
- “Can I still get electrolysis approved even if my state restricts gender-affirming care?”
Still, the answer is nuanced, and depends on the insurer’s national policy versus state-level implementation.
For example, here’s what Blue Cross in Massachusetts says about electrolysis insurance coverage.
1. National insurers with trans-inclusive policies
Companies like Kaiser, Blue Cross, Cigna, and Aetna maintain national guidelines for gender-affirming care, even if certain regions are less supportive.
If the national policy includes electrolysis under gender dysphoria treatment, approval is still possible.
Some clients in restrictive states have been approved for electrolysis in Washington or Oregon through out-of-state benefits because the insurer follows national rules.
2. Regional interpretations vary
Representatives in hostile states may:
- Lack training in gender-affirming care policy
- Default to classifying electrolysis as cosmetic
- Be unaware of national policy compliance requirements
This does not necessarily mean the care is excluded. It often means the representative is relying on limited information.
It’s also possible the representative has negative bias against transgender folks. Keep in mind that, while this might be due to actual transphobia, it could also be due to ignorance, misinformation, lack of life experience and/or familiarity with the subject and lack of exposure to actual trans folks.
While it would be understandable for you to take lack of cooperation, resistance or dismissal personally, consider that it is in your best interest to meet the moment with patience and grit. And who knows? You may be the agent of change who makes the path easier for the next trans person to interact with that insurance representative.
3. Strong documentation overrides incorrect verbal answers
When documentation is strong, many “verbally denied” cases are approved later.
4. Crossing state lines is sometimes covered
Insurers frequently approve electrolysis at out-of-state clinics when:
- Local clinics do not offer permanent removal
- Local clinics are not trans-competent
- The insurer’s national policy covers the service
- The state has weak protections but the plan itself is trans-inclusive
This is common with national carriers operating across restrictive regions.

What to Do If Insurance Says Electrolysis Is "Cosmetic"
When pursuing electrolysis insurance coverage, this is the most common obstacle people face. Representatives often default to “cosmetic” because they are reading from general procedure classifications instead of reviewing the gender-affirming care policy.
How to move the conversation in the right direction:
Here are some phrases that can get the insurance representative off their rote patterns and onto a more productive mindset:
- “My electrolysis is for gender dysphoria.”
- “This is part of my gender-affirming treatment plan.”
- “My surgeon requires permanent hair removal before surgery.”
Getting the electrolysis conversation 'unstuck'
If they still insist electrolysis is cosmetic, take these steps:
1. Ask for a written benefits clarification
Say: “Can you send documentation of this benefit determination in writing?”
Written responses often reflect actual rules more accurately than spoken ones.
2. Ask for a supervisor who handles medical necessity
Supervisors have access to detailed guideline manuals that call-center staff may not see.
3. Reference your diagnosis directly
Insurance systems route many benefits through diagnosis codes such as gender dysphoria.
4. Request that they check gender-affirming care guidelines
Many national insurers maintain trans-inclusive care standards even when local representatives are unaware of them.
5. Notify your providers
Clinics like Real You Electrolysis can help submit letters and appeals with appropriate language and documentation.
What to Do If Your Insurance Denies Electrolysis Coverage
Don’t panic!
A denial does not necessarily mean exclusion. Many denials are reversed after clarification or resubmission.
Common reasons for denials:
- Missing mental health letter
- Missing primary care letter
- Incorrect diagnostic code
- Outdated letter dates
- Representative error
- System error
- Lack of surgery confirmation when required
- Plan requiring preauthorization but none was submitted
Steps to take after a denial:
Request the denial letter in writing.
The written document explains the reason and cites plan policies.
Review the stated reason for denial.
Many are administrative, not policy-based.
Submit updated documentation.
Ensuring letters contain required language often resolves issues.
Have your surgeon reissue the requirement.
This is especially effective for vaginoplasty or phalloplasty prep.
Ask the insurer to review its national gender-affirming care policy.
This is useful for national carriers with inconsistent regional interpretations.
If needed, submit an appeal.
Appeals for pre-surgical genital electrolysis are commonly approved.
Why Some Plans Approve Electrolysis Insurance Coverage in OR/WA but Deny Elsewhere
States differ in their support for transgender healthcare
Washington and Oregon have some of the most trans-inclusive protections in the country. Medicaid programs in both states frequently cover electrolysis for:
- Facial hair removal
- Pre-surgical genital areas
- Graft sites
- Some torso or chest areas
Many states do not have equivalent protections, so representatives may be unfamiliar with coverage rules even when the insurer itself does cover the service.
The electrolysis insurance coverage decision structure looks like this:
- State-level rules determine what Medicaid must cover.
- Plan-level rules determine what private insurance must cover.
- National guidelines influence how multi-state carriers handle gender-affirming care.
A representative in a restrictive state might say “not covered,” while a representative in Washington might say “covered,” even for the same plan. While this might seem to be a policy contradiction, it’s really just a training issue.
Navigating Gender Dysphoria Documentation Requirements
Many clients ask us:
“What language must be included?”
“Does my provider need specific phrasing?”
“Do I need one letter or two?”
Core requirements appear consistently across insurers:
- Diagnosis of gender dysphoria
- Statement that electrolysis is part of gender-affirming care
- Identification of the specific areas needing treatment
- Explanation of medical necessity
- Confirmation that electrolysis supports functioning or surgical outcome
For vaginoplasty or phalloplasty prep, include:
- Direct reference to surgeon requirements
- Identification of scrotal area, perineum, mons, or graft sites
- Confirmation that permanent hair removal is required for safety
This removes ambiguity and accelerates approval.

Is Traveling for Electrolysis Covered by Insurance?
Many people in restrictive states ask whether insurance will cover treatment at clinics in Washington or Oregon.
The answer depends on the plan, but in many cases:
- Yes, out-of-state care is covered
- Yes, electrolysis at a clinic in Washington or Oregon can be approved
- Yes, insurers allow travel when the local area lacks competent providers
Examples of situations where out-of-state coverage is likely:
Many plans may approve travel for electrolysis hair removal in instances where:
- No local providers offer permanent electrolysis
- No providers have experience with trans patients
- No clinics perform pre-surgical genital electrolysis
Insurer’s national policy approves the service even if the local region discourages it
This is particularly common with Kaiser, Aetna, Blue Cross, and Cigna plans.
Patterns We See Across Major National Health Insurance Carriers
While policies differ by plan, many large carriers follow recognizable patterns in how they evaluate electrolysis as gender-affirming care. Understanding these patterns helps you anticipate approval likelihood.
Kaiser Permanente
Kaiser plans in Washington, Oregon, and California frequently approve:
Facial electrolysis
Pre-surgical genital electrolysis
Graft-site electrolysis
Approval tends to be consistent when documentation is complete. Some out-of-state Kaiser plans also approve treatment at clinics in Washington or Oregon when local providers are unavailable.
Blue Cross / Blue Shield
 Because BCBS is a network of state-level organizations, coverage varies.
Because BCBS is a network of state-level organizations, coverage varies.
However, BCBS affiliates that follow national gender-affirming guidelines often approve:
- Facial electrolysis for gender dysphoria
- Surgery preparation electrolysis
- Electrolysis at out-of-state clinics when medically aligned with guidelines
BCBS Illinois, for example, has approved electrolysis for clients treated in Washington and Oregon.
Aetna
 Aetna has increasingly recognized electrolysis as medically necessary for gender dysphoria and surgery preparation. Folks have a good shot of securing insurance approval for electrolysis with Aetna, especially when:
Aetna has increasingly recognized electrolysis as medically necessary for gender dysphoria and surgery preparation. Folks have a good shot of securing insurance approval for electrolysis with Aetna, especially when:
- A surgeon provides a clear requirement
- The client has a documented transition plan
- Diagnostic codes are current
Moda, Pacific Source, and OHP
 These insurers are widely used in Oregon and tend to support gender-affirming care.
These insurers are widely used in Oregon and tend to support gender-affirming care.
Moda, Pacific Source and OHP frequently approve:
- Facial electrolysis;
- Preparation for vaginoplasty and phalloplasty;
- Torso or graft-site electrolysis when medically supported.
Medicaid (in Oregon and Washington State)
Apple Health and Oregon Health Plan approve electrolysis hair removal more consistently than many private insurers.
Coverage usually includes:
- Facial electrolysis for gender dysphoria
- Genital surgery prep
- Graft-site preparation
- Some torso or chest areas
Medicare
As we mentioned earlier, Original Medicare excludes electrolysis across the board. Medicare Advantage coverage for electrolysis can have a bit of nuance though; some plans approve it when categorized under gender-affirming care.
How to Get Insurance to Approve Electrolysis: A Practical Guide

Clients often ask for a step-by-step method to maximize approval chances. Approval depends on showing medical necessity in clear, insurance-friendly language.
Below is a definitive strategy that reflects what works across insurers.
1. Get a current diagnosis of gender dysphoria
This is the foundational requirement across most carriers. Without it, electrolysis is usually classified as cosmetic by default.
2. Obtain two letters: mental health + primary care
Letters must:
- Be dated within the past 12–18 months
- Include diagnosis
- Identify the areas requiring electrolysis
- Explain its role in gender-affirming care
- Describe functional, emotional, or surgical impact
3. Secure a surgeon’s letter if you are preparing for surgery
Surgeon’s letters include this clear, standard language:
Permanent removal is required to ensure surgical outcomes.
This carries decisive weight.
4. Make sure the correct diagnostic codes are used
Some insurers still rely on outdated internal codes like F64.0, while others require updated ICD-10 gender dysphoria codes. Using the code the insurer expects reduces claim friction when interacting with insurance representatives and gatekeepers.
5. Ask the insurer to check the gender-affirming care policy
This bypasses default cosmetic classifications.
6. Request written confirmation of benefits
Written communication reduces errors and protects you during appeals.
7. Submit everything through a clinic that handles insurance regularly
Electrolysis clinics with experience in trans healthcare dramatically reduce approval delays by using correct procedural language and billing structures.
Checklist: What You Need Before Submitting an Insurance Request
Many of our clients want a simple checklist they can follow.
Use this list to ensure you meet common insurer requirements:
- Diagnosis of gender dysphoria
- Mental health letter with recommended treatment
- Primary care letter with medical necessity statement
- Surgeon’s letter (for vaginoplasty or phalloplasty prep)
- Identification of treatment areas (facial, scrotal, perineum, mons, graft sites, torso, chest)
- Correct diagnostic codes
- Clear treatment plan from the electrolysis provider
- Confirmation of whether preauthorization is required
- Written benefits summary from the insurer
Completing these steps increases approval consistency across all types of insurance.
How to Prepare for Your First Insurance-Covered Electrolysis Session
Once coverage is approved, people often ask what to expect next.
1. Understand the treatment areas
Facial electrolysis often begins with the upper lip, chin, jawline, and cheeks.
Surgery prep electrolysis usually focuses on:
- Scrotal area
- Perineum
- Mons pubis
- Graft sites such as forearm or thigh
2. Discuss session structure
Treatment plans vary depending on:
- Hair density
- Skin sensitivity
- Pain tolerance
- Area size
Depending on your skin type, schedule constraints and comfort level, sessions can last between 30 minutes to 2 hours. Facial hair removal may prove easier, which may allow for longer sessions. Genital areas can be especially sensitive, and shorter sessions may work better for that.
3. Ask about pain management options
Electrolysis on the scrotal area, perineum, or mons can be sensitive. At Real You Electrolysis, your comfort and safety matter. That’s why we partner with Lavender Spectrum Health. Many clients choose to stop in at Lavender to receive numbing injections prior to sessions involving sensitive regions.
These injections reduce pain, which allows for longer sessions. Pain management also supports emotional steadiness and improves overall treatment experience.
4. Ask how electrolysis insurance billing works
Your hair removal clinic should:
- Submit claims directly
- Track authorizations
- Update letters when required
- Support appeals if needed
Knowing that administrative work is handled supports peace of mind.
Emotional Realities of Electrolysis Coverage for Trans Women
Insurance navigation can be emotionally heavy. Many clients describe anxiety about misgendering by representatives, fear of being told electrolysis is cosmetic, stress over seeing outdated diagnostic codes, worry about exposing sensitive areas for treatment, and concern about pain during genital electrolysis.
Adding to the anxiety, many trans women fear that delays in permanent hair removal may postpone surgery.
These are not minor concerns. Facial hair can shape how the world interacts with you. Pre-surgical hair removal involves some of the most vulnerable areas of the body. The stakes are high, both emotionally and medically.
When clients arrive for electrolysis, many carry heavy emotions: Relief, grief, hope and/or emotional exhaustion.
Understanding these emotional layers is a critical part of trauma-informed care.
Why Trauma-Informed Electrolysis Matters
Electrolysis for gender-affirming care requires sensitivity and awareness. A trauma-informed electrolysis clinician recognizes the vulnerability of exposing sensitive areas, acknowledges the emotional weight tied to facial hair, understands the fear associated with pain in the scrotal area, perineum, or mons, and is aware of potential negative past experiences with medical staff, in settings that did not feel safe.
A trauma-informed electrologist:
- Uses affirming language
- Respects boundaries throughout the session
- Explains each step clearly
- Checks in frequently
- Allows clients to pause as needed
- Supports autonomy
This approach helps clients move through treatment with dignity and confidence.
Some Frequently-Asked Questions About Insurance Coverage for Electrolysis
Here are some of the most common questions we get at Real You Electrolysis, paired with direct answers:
Can I get electrolysis covered if I’m not transitioning?
Insurance coverage for hair removal is tied to medical necessity. For most insurance plans, electrolysis is only covered when associated with gender dysphoria or preparing for gender-affirming surgery.
Non-transition-related electrolysis is rarely covered.
That said, if you have a serious skin condition, such as HS or folliculitis, or a hormonal condition such as PCOS, it may be worth a few phone calls to find out if you can get insurance coverage for your hair removal treatments.
Does insurance cover electrolysis hair removal for nonbinary people?
Yes, when medically necessary for gender dysphoria or surgical preparation. Coverage is based on diagnosis and treatment purpose, not identity labels.
Will insurance cover electrolysis for body hair?
Sometimes.
If torso or chest hair removal reduces dysphoria or supports surgical preparation, insurers may approve it with strong documentation.
Is electrolysis covered for transgender men?
Yes, when preparing for phalloplasty or other procedures requiring graft-site preparation.
Coverage can also apply to facial or body areas when treating gender dysphoria.

Your Next Step Toward Permanent Hair Removal
Insurance-covered electrolysis is within reach for many trans women, trans men, and nonbinary people. When documentation is strong and your care team understands how insurers operate, approvals become far more predictable.
You might feel hesitant.
You might feel unsure about calling your insurer.
You might feel nervous about exposing sensitive areas for surgery prep hair removal.
You might feel concerned about pain management.
You might feel worried about navigating the maze of insurance plans.
You might fear being misunderstood by medical staff.
These are real experiences.
This is why our practice was created.
You deserve care that removes these barriers.
Just Imagine!
Imagine appointments that feel more like self-care than a medical chore
Imagine getting the final ok for surgery, and a date for your procedure.
Imagine the gender euphoria of feeling smooth skin on your face.
What It Feels Like at Real You Electrolysis
- You get to feel comfortable and cared for throughout all your electrolysis treatments.
- You do not have to worry about being the only trans person in the space.
- Your treatments will be most likely covered by insurance.
- You will have minimal or no costs out of pocket.
- You achieve permanently hair-free skin.
At our clinics, you get comprehensive support
When you choose Real You Electrolysis, you receive more than a service.
Patients have called our practice a home away from home.
Clients have raved about our electrologists and staff.
This is what you get at our clinics:
- A queer-centric team experienced in navigating gender-affirming care
- Trauma-informed, queer-friendly, trans-affirming treatment environments
- A clear plan for facial electrolysis, surgery prep electrolysis, or graft-site treatment